The Science Your Surgical Team May Not Tell You—And How to Prepare Your Brain and Body
If you’re a woman in your late 30s to early 50s facing surgery, there’s something important your surgical team probably won’t mention: your hormones are changing in ways that can make anesthesia recovery harder.
This isn’t about being “over 40” or “getting older.” It’s about specific biological shifts that affect how your brain handles stress, clears medications, and bounces back from the inflammatory hit of surgery.
And here’s the good news: once you understand what’s happening, you can do something about it.
Why Some Women Struggle More After Surgery
Doctors call it “postoperative cognitive dysfunction” or POCD. You might call it brain fog that doesn’t lift, memory problems that linger, or just not feeling like yourself for weeks or months after surgery.
Research published in the International Urogynecology Journal (2020) found that 33% of women over 60 experienced cognitive problems after pelvic surgery—that’s one in three women. The researchers identified key risk factors: women who were already dealing with depression or frailty before surgery were significantly more vulnerable.
What does this tell us? The brain doesn’t get foggy because of the anesthesia alone. It gets foggy because it didn’t have enough reserve to handle the stress.
This is the core insight that changes everything. If low reserve is the problem, then building reserve is the solution—and perimenopause is quietly draining that reserve in multiple ways.
The Neuroinflammation Connection: What’s Actually Happening in Your Brain
Surgery doesn’t just happen to your body—it triggers a systemic inflammatory response that reaches your brain. Understanding this mechanism helps explain why some women are more vulnerable than others.
Research published in Nature Immunology (2020) and Anesthesia & Analgesia (2019) has mapped out how this happens:
- Surgical trauma triggers peripheral inflammation
- Pro-inflammatory cytokines—especially IL-6—surge in the bloodstream
- IL-6 signaling increases blood-brain barrier permeability
- Inflammatory mediators enter the brain, activating microglia and disrupting neural function
In simple terms: surgery creates inflammation throughout your body, and that inflammation can “leak” into your brain through a compromised blood-brain barrier.
The clinical significance is clear: patients with higher baseline inflammation or reduced capacity to resolve inflammatory signaling are at greater risk for cognitive complications.
This is where perimenopause becomes relevant. The hormonal shifts you’re experiencing don’t just affect your mood or sleep—they directly impact your brain’s ability to manage this inflammatory cascade.

Progesterone: Your Brain’s Natural Protector Is Declining
Most women know about estrogen decline during menopause. But progesterone actually starts dropping earlier—often in your mid-to-late 30s—and this matters more for brain protection than most people realize.
Think of progesterone as your brain’s natural calming and protective agent. It’s like going into a storm with a thinner umbrella—when progesterone is low, your brain has less natural protection against the inflammatory stress that comes with surgery.
But the science goes deeper than that analogy suggests. Progesterone and its metabolite allopregnanolone function as neurosteroids with direct neuroprotective properties. Research in the Journal of Steroid Biochemistry and Molecular Biology (2015) and Acta Pharmacologica Sinica (2013) documents how progesterone:
- Reduces neuroinflammation by regulating microglial activation and cytokine production
- Supports myelin repair and oligodendrocyte function (critical for nerve signal transmission)
- Enhances mitochondrial function and reduces oxidative stress via the PI3K/Akt pathway
- Modulates GABA-A receptors through allopregnanolone, providing anxiolytic and neuroprotective effects
Research in Frontiers in Endocrinology (2024) further shows that allopregnanolone enhances mitochondrial respiration and supports synaptic recovery. When progesterone declines, you lose this entire protective cascade—leaving your brain more vulnerable to surgical stress.
The Estrogen-Histamine Connection: Why You React Differently Now
Here’s something that surprises many women: during perimenopause, estrogen doesn’t just decline—it fluctuates wildly. And those high estrogen spikes can trigger a cascade of histamine problems that affect how you respond to medications, including anesthetics.
Research published in Frontiers in Immunology (2012) demonstrated that estrogen directly activates mast cells—the immune cells that store and release histamine. The mechanism involves estrogen-induced calcium influx into mast cells, triggering degranulation and histamine release. Evidence also suggests estrogen may downregulate diamine oxidase (DAO), the primary enzyme responsible for histamine degradation.
This creates a problematic feedback loop:
- Estrogen spikes → mast cell activation → histamine release
- Histamine → stimulates aromatase → more estrogen production
- More estrogen → more mast cell activation → more histamine (cycle amplifies)
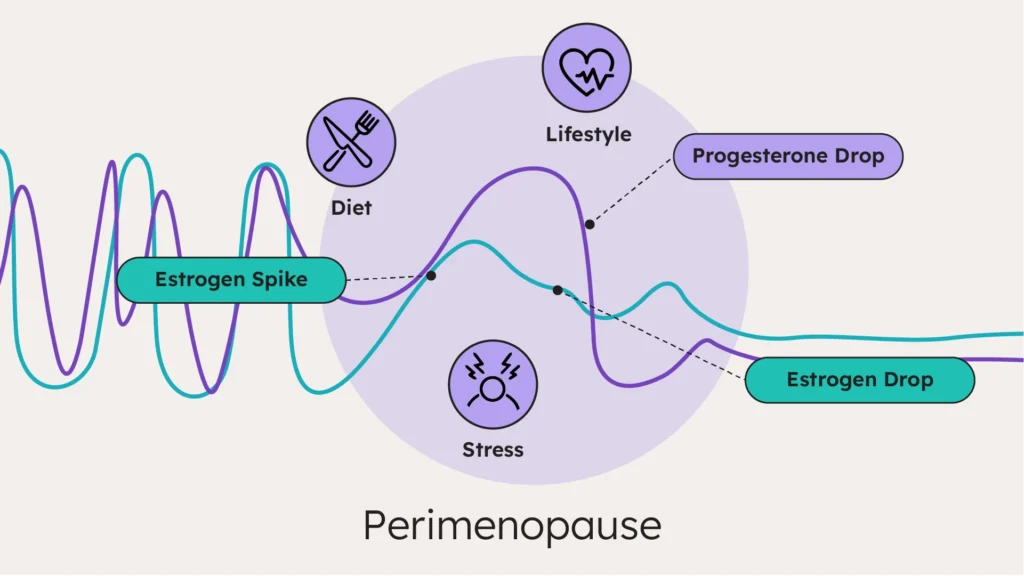
Meanwhile, progesterone normally helps stabilize mast cells and reduce histamine release—but it’s declining. So you’ve got more histamine being released and less natural braking system.
What does this mean for surgery? Some anesthetic agents can elevate histamine levels. If you’re already dealing with histamine intolerance—new food sensitivities, headaches, flushing, itching, worsening anxiety, or unusual reactions to medications—your body may respond more strongly to certain anesthetics and recover more slowly.
Methylation and Detoxification: The Hidden Challenge
Your liver is responsible for clearing anesthetic drugs, processing the byproducts of surgical stress, and metabolizing your fluctuating hormones. That’s a substantial workload—and perimenopause makes it harder.
Research shows that hepatic blood flow decreases by approximately 1% per year after age 40. At the same time, declining estrogen reduces the liver’s antioxidant protection and regenerative capacity. Your detoxification capacity is shrinking right when the demands on it are increasing.
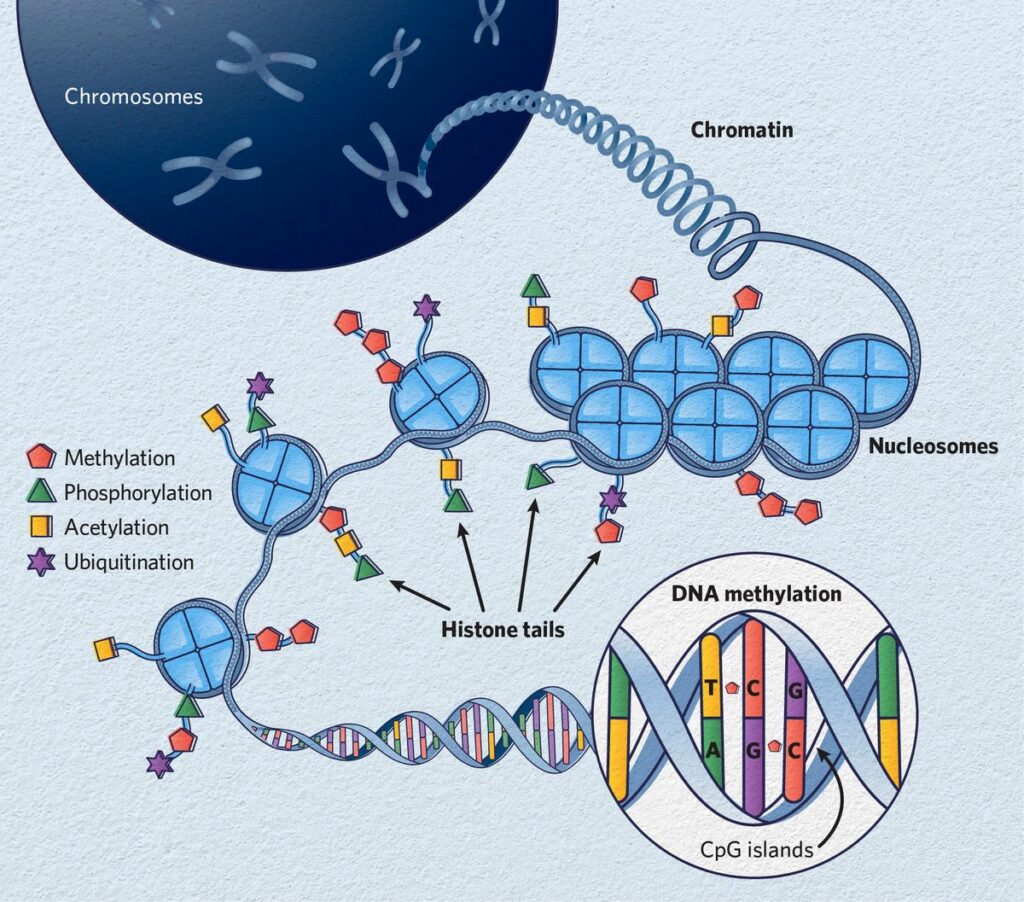
Here’s where methylation becomes critical. Methylation is a biochemical process—the transfer of methyl groups (CH₃) to substrates throughout the body—that your system uses to:
- Conjugate and clear estrogen through Phase II hepatic detoxification (COMT pathway)
- Synthesize neurotransmitters including serotonin, dopamine, and norepinephrine
- Support DNA repair and cellular regeneration
- Regulate stress hormone metabolism and HPA axis function
Up to 40% of the population has genetic polymorphisms in the MTHFR gene that can reduce methylation efficiency by up to 70%. A study in Maturitas (2008) found that these MTHFR variations were more strongly correlated with depression in postmenopausal women—suggesting that methylation challenges become clinically significant as hormonal demands on the pathway increase.
During perimenopause, methylation is under increased demand: clearing fluctuating estrogen, supporting neurotransmitter synthesis during hormonal shifts, and managing elevated stress hormone turnover. Add surgical stress to this equation, and the system can become overwhelmed.
Cortisol Dysregulation: When Stress Recovery Takes Longer
Your stress response system—the hypothalamic-pituitary-adrenal (HPA) axis—is supposed to surge when needed, then calm back down. But perimenopause can disrupt this regulation in ways that compromise your recovery capacity.
A study in Menopause (2020) found that women with severe vasomotor symptoms (hot flashes) had altered cortisol awakening response (CAR) patterns. Specifically, those with the most symptoms showed only a 30% cortisol increase upon waking, compared to 67% in women with fewer symptoms.
That might sound backwards—isn’t less cortisol better? Not in this context. A blunted cortisol awakening response indicates HPA axis dysregulation—a pattern associated with reduced stress adaptation capacity and impaired recovery from acute stressors.
Research in the American Journal of Psychiatry (2015) and Frontiers in Endocrinology (2023) suggests that fluctuating neurosteroids—including the allopregnanolone we discussed earlier—may compromise GABA-A receptor plasticity, exacerbating stress response dysregulation during perimenopause.
Surgery is one of the most significant acute stressors your body can experience. If your HPA axis is already dysregulated—running on empty, unable to mount an appropriate response and then recover—surgical stress takes longer to resolve and the cognitive effects linger.
Oxidative Stress and Antioxidant Depletion
Glutathione is your body’s master antioxidant—the primary defense system protecting your cells from oxidative damage, supporting detoxification, and maintaining brain function. Unfortunately, perimenopause depletes it.
Research in Maturitas (2015) documented that perimenopausal and postmenopausal women show decreased levels of key antioxidants including α-tocopherol (vitamin E) and retinol (vitamin A), alongside increased markers of oxidized glutathione. A follow-up study in the Bulletin of Experimental Biology and Medicine (2022) confirmed that postmenopausal women had significantly lower glutathione reductase activity and a compromised GSH/GSSG ratio—the balance between protective reduced glutathione and its oxidized form.
Why does this matter? Glutathione is essential for Phase II hepatic conjugation—the process that makes anesthetic drugs and their metabolites water-soluble for elimination. It’s also critical for neutralizing the reactive oxygen species generated by surgical inflammation and protecting neurons from oxidative damage.
Estrogen itself has antioxidant properties that protect tissues during high-oxidative-stress states. When estrogen fluctuates and eventually declines, you lose some of this protective capacity. Surgery creates a massive oxidative hit—and if your antioxidant reserve is already depleted, recovery is compromised before you even reach the operating room.
Seeing the Bigger Picture: Why Assessment Matters
If you’ve read this far, you can see that perimenopause doesn’t create just one challenge—it creates overlapping vulnerabilities that compound each other. Declining progesterone reduces neuroprotection. Estrogen fluctuations trigger histamine cascades. Methylation becomes overburdened. The HPA axis dysregulates. Antioxidant capacity drops.
This is why standard preoperative evaluation often misses the mark for perimenopausal women. The traditional question—”Are you sick enough to postpone surgery?”—doesn’t capture what’s actually happening.
A better question is: “How much stress can this nervous system absorb right now—and where are the specific bottlenecks?”
The Neuro-Resilience Index™
This is the foundation of my clinical approach: the Neuro-Resilience Index™ (NRI™)—an assessment framework designed to measure neurologic reserve and identify specific vulnerabilities before they become problems. NRI™ doesn’t prescribe—it classifies. It tells you where your system is fragile, so you can target your preparation accordingly.
More on the NRI™ is coming soon. For now, let’s focus on what you can do once vulnerabilities are identified.
The HARP™ Framework: Preparing Your Brain and Body
What is HARP™?
HARP™ (Holistic Anesthesia Prep and Recovery) is a clinical framework for supporting your nervous system through surgical stress. Once you understand where your vulnerabilities lie, HARP™ provides the roadmap for what to do about them.
H – Health Assessment (identifying your specific vulnerabilities)
A – Assess Environmental Stressors (load and drains on your reserve)
R – Resilience Building (strengthening your system before the stress)
P – Post-Op Recovery (supporting the system after the stress)
Based on the perimenopause-specific vulnerabilities we’ve discussed, here’s how the HARP™ framework applies. Important: Always discuss supplements and lifestyle changes with your healthcare team before surgery—some may need to be discontinued 1-2 weeks prior.
Support Your Methylation Pathways
Why it matters: Methylation supports estrogen clearance through COMT-mediated conjugation, neurotransmitter synthesis via SAMe (S-adenosylmethionine) pathways, and detoxification capacity—all under increased demand during perimenopause and surgical recovery.
What to do:
- Prioritize dietary folate: dark leafy greens, asparagus, avocado, lentils, and liver provide bioavailable forms
- Include choline-rich foods: eggs (especially yolks), organ meats, and cruciferous vegetables support phosphatidylcholine synthesis and methyl donation
- Consider methylated B vitamins: L-methylfolate (5-MTHF) and methylcobalamin bypass MTHFR enzyme limitations if you have known polymorphisms
- Ensure adequate magnesium: this mineral serves as a cofactor for COMT and numerous methylation-dependent enzymes
Optimize Liver Detoxification
Why it matters: Your liver processes anesthetic drugs through Phase I (CYP450 oxidation) and Phase II (conjugation) pathways, clears surgical inflammation, and metabolizes fluctuating hormones. Supporting all three phases of detoxification optimizes drug clearance and recovery.
What to do:
- Eat cruciferous vegetables daily: broccoli, cauliflower, Brussels sprouts, and cabbage contain DIM (diindolylmethane) and sulforaphane, which support healthy estrogen metabolism through the 2-OH pathway
- Reduce hepatic burden: minimize alcohol and ultra-processed foods in the weeks before surgery to preserve detoxification capacity for anesthetic clearance
- Support Phase III elimination: adequate fiber (25-35g daily), hydration, and regular bowel movements ensure conjugated toxins and hormones are eliminated rather than reabsorbed through enterohepatic recirculation
Address Histamine Sensitivity
Why it matters: Elevated histamine levels can amplify reactions to certain anesthetic agents and compromise recovery. Identifying and addressing histamine intolerance before surgery reduces this risk.
What to do:
- Track your symptoms: new food sensitivities, headaches, flushing, itching, or unusual anxiety may indicate histamine intolerance—keep a symptom diary to identify patterns
- Support DAO enzyme activity: diamine oxidase requires pyridoxal-5-phosphate (active B6), vitamin C, copper, and zinc as cofactors for histamine degradation
- Communicate with your anesthesiologist: if you suspect histamine sensitivity, inform your anesthesia provider—they can select agents with lower histamine-releasing potential and adjust your protocol accordingly
Build Your Antioxidant Reserve
Why it matters: Surgery generates substantial reactive oxygen species. Robust antioxidant capacity—particularly glutathione—supports Phase II hepatic conjugation, neutralizes oxidative damage, and protects neural tissue during recovery.
What to do:
- Eat sulfur-rich foods: garlic, onions, and cruciferous vegetables provide cysteine and other precursors for endogenous glutathione synthesis
- Consider NAC supplementation: N-acetyl cysteine is a well-researched glutathione precursor with documented neuroprotective effects and support for hepatic detoxification pathways
- Include colorful produce: the polyphenols and carotenoids in deeply pigmented fruits and vegetables provide additional antioxidant and anti-inflammatory support
- Ensure adequate vitamins C and E: these work synergistically with glutathione to regenerate antioxidant capacity
Regulate Your Stress Response
Why it matters: HPA axis dysregulation compromises your capacity to mount an appropriate stress response and recover from acute stressors. Building stress resilience before surgery supports faster, more complete recovery.
What to do:
- Prioritize sleep hygiene: maintain consistent sleep-wake times to support circadian cortisol rhythm; limit evening light exposure to protect melatonin production
- Practice vagal toning: deep diaphragmatic breathing, meditation, or gentle yoga activate parasympathetic pathways and help regulate HPA axis function—even 10 minutes daily shows benefit
- Consider adaptogenic support: ashwagandha (Withania somnifera) has research supporting HPA axis modulation—discuss timing of discontinuation with your provider before surgery
- Get morning light exposure: bright light within the first hour of waking helps anchor circadian rhythm and supports healthy cortisol awakening response
You’re Not Imagining It
If you’ve felt like something is different about how you respond to stress, medications, or recovery—you’re probably right. Perimenopause changes the landscape of your nervous system in ways that mainstream medicine is only beginning to understand and address.
But here’s what’s empowering: you don’t have to wait for your surgical team to catch up.
You can understand your vulnerabilities. You can apply the HARP™ framework to build your reserve. And you can enter surgery with a brain and body that’s prepared—not just medically cleared, but genuinely ready for the stress ahead.
That’s the difference between hoping for a good outcome and actively creating the conditions for one.
Want to go deeper?
My upcoming book, Break Through Anesthesia Fog, provides a complete guide to understanding neurologic reserve, applying the HARP™ framework, and preparing your brain and body for surgical stress—including detailed protocols for perimenopausal women. Join the presale list to be notified when it launches.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult with your healthcare team before making changes to your surgical preparation plan. Some supplements may need to be discontinued before surgery—discuss timing with your provider.
About the Author
Sande Bargeron, PA-C, CAA, PhD is a brain health optimization expert and the creator of the Neuro-Resilience Index™ and HARP™ framework. With decades of experience in anesthesia and a commitment to translating complex neuroscience into actionable clinical strategies, she helps patients and practitioners prepare for surgical stress—and build lasting neurologic resilience.
