The Hidden Brain Crisis No One Warns You About Before Surgery
Understanding Postoperative Delirium, Building Cognitive Reserve, and Protecting Your Brain Before Major Surgery
By Sande Bargeron | Neuro Resilience Expert & Brain Health Optimization Specialist
One in four adults over 65 will experience delirium after major surgery.
In some patients—particularly those undergoing cardiac or hip fracture surgery—that number climbs to nearly one in two.
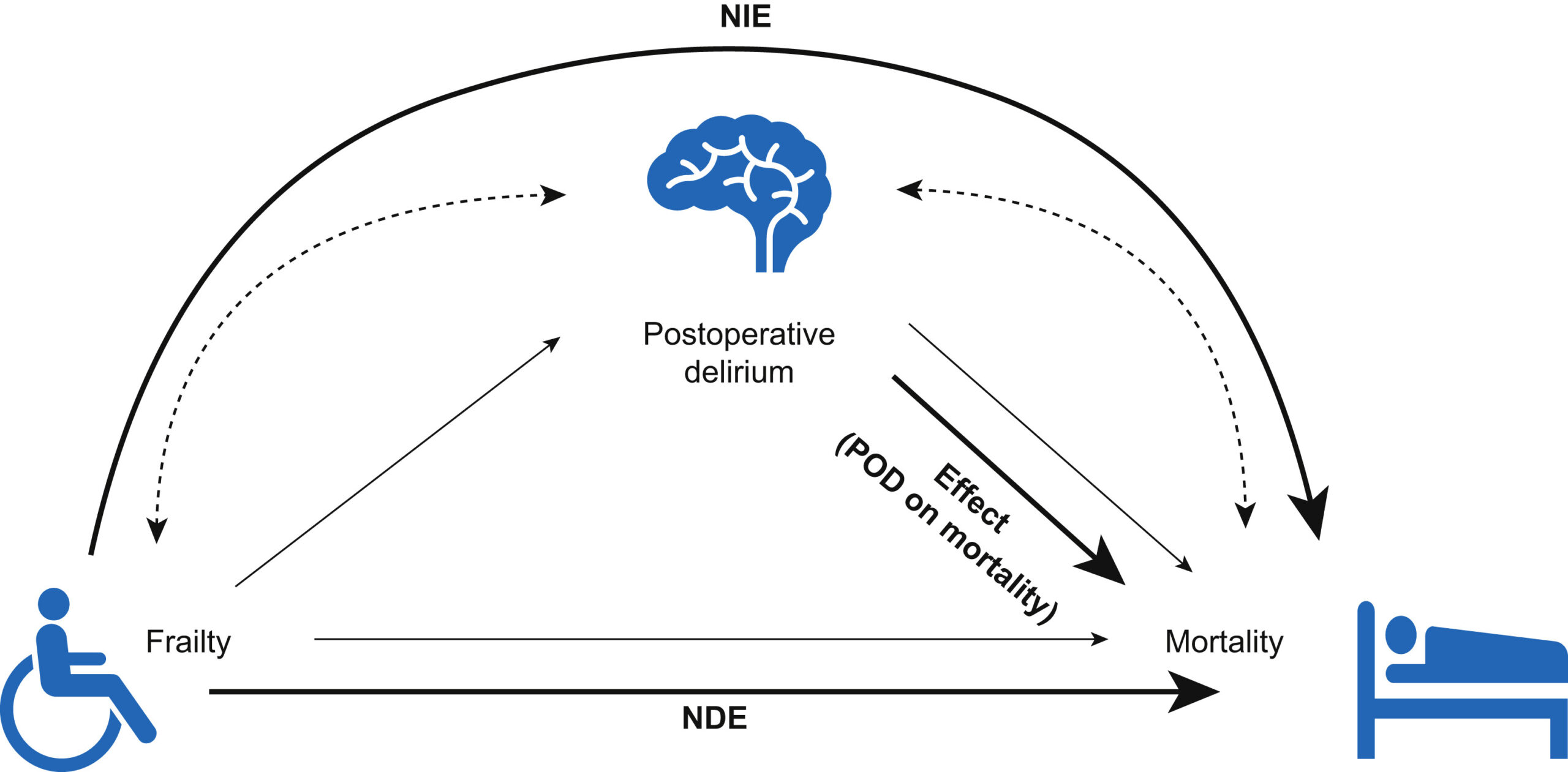
This is not a minor inconvenience. Research shows that postoperative delirium is linked to 40% faster cognitive decline. Multiple studies demonstrate it increases dementia risk two to five-fold. And yet, most patients have never heard the word “delirium” mentioned in their preoperative conversations.
What if we could see vulnerability before surgery—and do something about it?
What Is Postoperative Delirium?
Delirium is a sudden, acute disturbance in attention, awareness, and cognition. It typically emerges within hours to days after surgery and manifests in ways that can be deeply distressing for patients and families alike.
Common presentations include:
- Confusion about time, place, or identity
- Visual or auditory hallucinations
- Fluctuating levels of consciousness
- Agitation or, conversely, unusual lethargy
- Memory gaps for the episode itself
Crucially, delirium is not random. It does not simply happen because of anesthesia. It does not occur in a vacuum. Delirium is the brain revealing what was already running low—a window into depleted cognitive reserve that the stress of surgery exposed.
The Cognitive Reserve Framework: Why Some Brains Weather the Storm
Cognitive reserve refers to the brain’s capacity to cope with damage or stress while maintaining function. Think of it as the brain’s resilience buffer—the difference between a system that can absorb shock and one that fractures under pressure.
Key Research Finding
The groundbreaking Neurobics Trial published in JAMA Surgery demonstrated that preoperative cognitive exercise—tablet-based brain training targeting memory, speed, attention, flexibility, and problem-solving—reduced postoperative delirium rates from 23% to 13.2% in patients who completed the training protocol.
This is not theoretical. This is measurable. And most importantly, it is actionable.
Why Your Doctor Doesn’t Warn You
The current medical system is built around a fundamental question: “Are you sick enough to postpone surgery?”
It is not designed to ask:
“Is your brain ready to handle this stress?”

Before surgery, your heart gets checked. Your lungs get evaluated. Your labs get reviewed. But your brain’s reserve—the very thing that determines whether you’ll emerge cognitively intact—remains largely invisible in standard preoperative protocols.
This is changing. The European Society of Anaesthesiology’s 2024 guidelines now recommend comprehensive geriatric assessment evaluating frailty, sensory impairment, malnutrition, and cognitive function before elective surgery. But implementation remains inconsistent, and the burden often falls on patients and families to advocate for proactive brain protection.
The Science of Prevention: What Actually Works
The most robust evidence for delirium prevention comes from multicomponent non-pharmacological interventions—bundled strategies that address multiple risk factors simultaneously.
The AKTIVER Delirium Prevention Program
A landmark 2022 stepped-wedge cluster randomized controlled trial published in JAMA Surgery followed 1,470 patients aged 70 and older undergoing elective non-cardiac surgery. The intervention included daily multicomponent, patient-centered care: cognitive stimulation, orientation protocols, early mobilization, sleep optimization, sensory aids, medication review, and family involvement.
Result
33% relative reduction in delirium incidence and fewer total delirium days following general and orthopedic surgery.
The Hospital Elder Life Program (HELP)
The foundational HELP protocol demonstrated a 40% reduction in delirium incidence through systematic implementation of orientation support, early mobilization, hydration optimization, sleep protocols, and sensory correction.
Meta-analyses pooling multiple randomized and non-randomized trials show multicomponent interventions reduce delirium incidence with an odds ratio of 0.46—meaning these strategies roughly cut delirium risk in half.
Circadian Rhythm and Sleep: The Overlooked Vulnerability
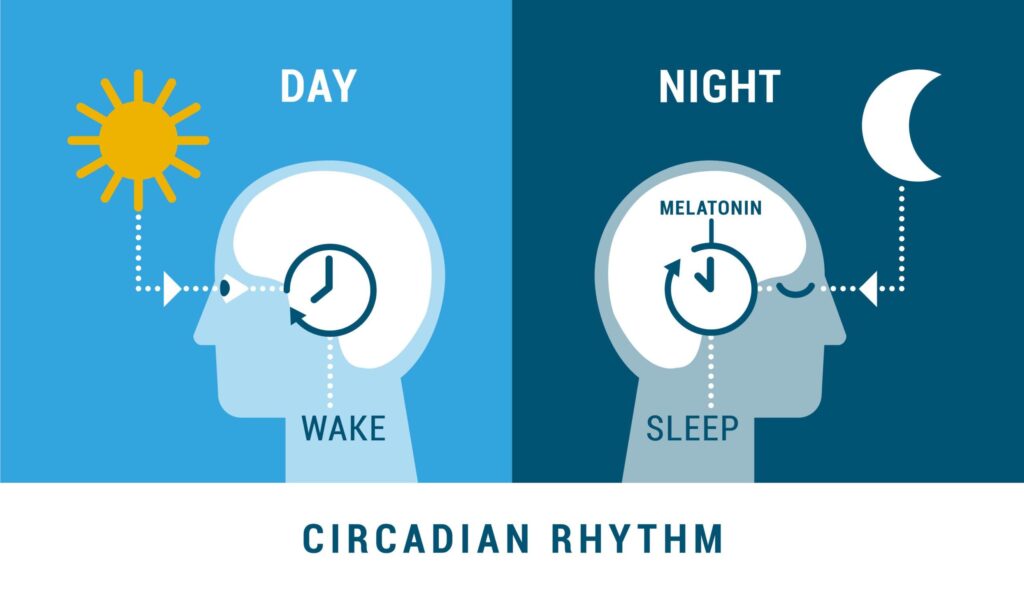
A 2019 systematic review and meta-analysis found that sleep and circadian interventions were associated with a 52% reduction in postoperative delirium risk (pooled RR = 0.48). The pooled delirium incidence dropped from 20.7% in control groups to 8.6% in intervention groups.
What disrupts circadian health around surgery:
- Hospital environments with constant artificial light
- Fragmented sleep from vital sign checks and monitoring
- Anesthesia’s suppressive effects on clock gene expression
- Surgery-induced inflammation disrupting melatonin rhythms
Research published in Frontiers in Neuroscience (2024) describes how circadian-effective lighting—bright daytime exposure and dim nighttime conditions—can resynchronize abnormal rhythms and protect cognitive function.
Your Actionable Pre-Surgery Brain Protection Protocol
Based on the highest-quality clinical evidence, here are the non-pharmacological strategies you can implement:
1. Cognitive Prehabilitation (2-4 Weeks Before Surgery)
What it is: Structured brain exercises targeting memory, attention, processing speed, and cognitive flexibility.
Evidence: The Neurobics Trial showed patients who completed cognitive exercises had a 43% lower delirium rate (13.2% vs 23.0%).
How to implement: Aim for 10+ hours of brain training before surgery. Use validated platforms targeting multiple cognitive domains. Even partial completion showed benefit.
2. Sleep Optimization (Start 1-2 Weeks Before Surgery)
What it is: Establishing robust sleep-wake patterns and addressing underlying sleep disturbances.
Evidence: Preoperative sleep disruption independently predicts postoperative delirium. Patients who developed delirium had significantly longer nighttime awakenings before surgery.
How to implement: Maintain consistent sleep-wake times. Get bright light exposure within 1 hour of waking. Avoid screens 2 hours before bed. Keep the bedroom cool, dark, and quiet.
3. Circadian Entrainment Protocol
What it is: Strengthening your body’s natural 24-hour rhythms before and during hospitalization.
Evidence: Timed bright light exposure reduces postoperative delirium. Reducing ambient light and noise at night improves sleep quality and decreases delirium incidence.
How to implement: Spend 30+ minutes in bright outdoor light each morning. After surgery, advocate for window beds and request that non-essential lighting be dimmed after sunset.
4. Nutritional Optimization for Brain Resilience
What it is: Ensuring adequate intake of nutrients that support neurological function and recovery.
Evidence: Malnutrition is a known delirium risk factor. Omega-3 fatty acids (particularly DHA, comprising 97% of brain fatty acids) support cognitive function. Vitamin D deficiency affects nearly 95% of brain injury patients.
How to implement: Prioritize fatty fish 2-3 times weekly. Include protein at every meal. Consume colorful vegetables and berries. Ensure adequate vitamin D. Stay well-hydrated.
5. Physical Prehabilitation
What it is: Structured exercise before surgery to improve overall functional reserve.
Evidence: Multimodal prehabilitation reduces postoperative complications including delirium. Animal studies show preoperative environmental enrichment attenuates surgery-induced neuroinflammation.
How to implement: Begin a structured walking program 2-4 weeks before surgery. Include resistance exercises if cleared by your physician. Continue gentle mobilization early after surgery.
6. Sensory Optimization
What it is: Ensuring vision and hearing are optimized before and throughout hospitalization.
Evidence: Sensory impairment is a modifiable delirium risk factor included in all major prevention protocols.
How to implement: Get vision and hearing tested before surgery. Bring glasses and hearing aids to the hospital. Keep backup batteries for hearing aids.
7. Family Involvement and Orientation Support
What it is: Active participation of family members in cognitive support and reorientation.
Evidence: A 2025 systematic review found family involvement significantly prevents delirium. Reorientation alone can reduce overt delirium by 40%.
How to implement: Designate a family member to be present consistently, especially first 72 hours post-surgery. Bring familiar objects. Gently reorient to time, place, and situation.
The Paradigm Shift: From Reaction to Prevention
For too long, we have accepted delirium as an unfortunate but unavoidable complication of surgery in older adults. The evidence tells a different story. Research consistently demonstrates that 30-40% of delirium cases are preventable through systematic multicomponent interventions.
Delirium is not a sign that something went wrong with surgery. It is a sign that the brain did not have enough reserve to handle the stress. And that distinction matters profoundly—because reserve is something we can measure, and it is something we can build.
What if, instead of finding out your brain was vulnerable after something went wrong, you could see it clearly beforehand—and do something about it?
That is the question I have been building toward. In upcoming content, I will show you what measuring cognitive reserve actually looks like—and how we can use that knowledge to protect the brains of those we love before they face their next surgical challenge.
Your Next Step
If you or a loved one has surgery scheduled, start the conversation with your medical team about delirium prevention protocols. Ask what multicomponent interventions are available at your hospital. And begin implementing the prehabilitation strategies outlined above today.
Disclaimer: This content is for educational purposes only and does not constitute medical advice. Always consult with your healthcare providers before making changes to your medical care or implementing new health protocols.
Sande Bargeron is a brain health optimization expert and neuro resilience specialist dedicated to translating cutting-edge neuroscience research into actionable strategies for cognitive protection and recovery.
